CQC’s State of Care report: What it Means for Social Care
The urgent call for help is clear. This year’s Care Quality Commission (CQC) State of Care Report provides a stark assessment of increasing pressures on our social care system. Here's what you need to know.
6 minute read
Staff shortages and the ongoing struggle to recruit and retain staff are some of the largest challenges faced across the health and care sectors. Our Big Exit Interview report found that 1 in every 10 health and social care service workers could leave the sector this year.
Many of the key findings in the latest CQC’s annual assessment also point to a critical lack of government funding, which is affecting all areas of the health and social care systems.
Among the gloomy findings, there is some good news: the quality of care is reported to be mainly 'good or outstanding' despite the administrative chaos and the ongoing workforce crisis.
The report also concludes that there is some hope: the gridlock which has paralysed the system could be gradually eased with the help of new, innovative solutions which help to optimise workflow.
Blog highlights:
- The health and social care system remains backlogged. 1 in 5 people (22%) are awaiting healthcare services, with unacceptable waiting times for care assessment, vast backlogs of elective appointments and blocked patient flow.
- Workforce shortages are chronic, with more than 9 in 10 NHS leaders warning of a social care workforce crisis in their area. Figures show that 87% of care home providers and 88% of home care providers are currently experiencing recruitment challenges.
- Working conditions in the health and social care systems are, in some cases, so bad they are affecting care workers’ abilities to carry out their work. Only 43% of NHS staff feel they can meet all the conflicting demands on their time at work. Similarly, care services are facing sky-high vacancy rates of up to 160,000 positions, creating conditions which are simply incompatible with rising demand and insufficient funding.
- Care quality and accessibility is significantly lower for ethnic minorities, people with disabilities, and those who live in deprived areas. Those with learning disabilities and people with autism also face huge inequalities when accessing health and social care. Local councils are left to deal with increasing requests for help while social care capacity actively reduces, and the number of carers steadily decreases.
We look at some of those points in more detail below.
 A gridlocked system that is leaving patients and staff dissatisfied
A gridlocked system that is leaving patients and staff dissatisfied
A care system can only function if there is good patient flow and sufficient resources available to meet the demand for services.
The gridlocked system described in the report compromises both patient safety and the safety of the entire system, staff included.
This standstill is an issue of high urgency due to its serious knock-on effects, including:
Unsatisfactory conditions are resulting in high staff turnover
A major contributing factor to this standstill is the care workforce crisis, which 99% of NHS leaders believe is affecting their area.
Care homes with nursing had the highest sickness rates of 8.2 days, almost twice the pre-pandemic rate of 4.8 days. The average number of sick days in non-nursing care homes and homecare services was lower but still higher than pre-pandemic levels.
Staff vacancy levels are also now higher than they were before the pandemic, and the highest they have been for five years.
Increasing staff retention in the Social Care system is essential. During the first three months of 2022, 2.2 million hours of homecare could not be delivered because of insufficient workforce capacity.
High turnover is closely associated with high levels of employee dissatisfaction, and widespread post-pandemic burnout.
In our Big Exit Interview report, the two most-selected reasons for leaving among our 1,000 survey respondents working in social care were low pay and overwork.
These factors usually create a vicious cycle: employees feel like they’re going above and beyond and then receive minimal or no recognition.
Improving pay and conditions remains a huge challenge in care, but everything that can be done must be done to address the current workforce crisis.
There’s not enough funding for the social care industry
This isn’t news, of course, but now more than ever, the government needs to invest in the health and care system, both in terms of funding and attention. Overall, patient care is at a ‘good or outstanding’ level, but at a very high cost to staff wellbeing.
Councillor David Fothergill, Chairman of the Local Government Association’s Community Wellbeing Board said: “Social care needs £13 billion of additional funding to address the long and short-term challenges the sector is facing. There needs to be immediate investment to end this gridlock.”
Without more money and long-term Social Care reform, it’s hard to see how providers can address the biggest workforce issue of all - pay rates.
There’s an unacceptably long wait for social care
Half a million people are waiting either for an adult social care assessment, for a care payment to begin, or for a review of their care.
Reducing this wait time needs to be a priority: of those waiting for a care needs assessment, 40% said that their ability to carry out day-to-day activities was now worse than when the assessment was requested.
These eye-popping figures might seem shocking, but they’re nothing new. The backlog of elective appointments and delay in social care assessment has only increased during successive governments and continues to do so.
Social care staff are not to blame: rising demand and staffing issues are behind these waiting times.
However, these delays are placing families or unofficial carers under mounting pressure, and increasing feelings of anxiety among those awaiting care as needs increase over time. In fact, the number of people giving substantial unpaid care has risen by 42% since the height of the pandemic, with caregivers’ health, well-being and paid work suffering.
 Innovative workforce solutions are emerging to help tackle the industry’s biggest problems
Innovative workforce solutions are emerging to help tackle the industry’s biggest problems
While there is significant cause for concern throughout the system, the report also highlights the potential for positive change. The implementation of integrated care systems (ICSs) provides an opportunity to better identify good or poor quality of care, particularly in the local care systems, and make necessary changes.
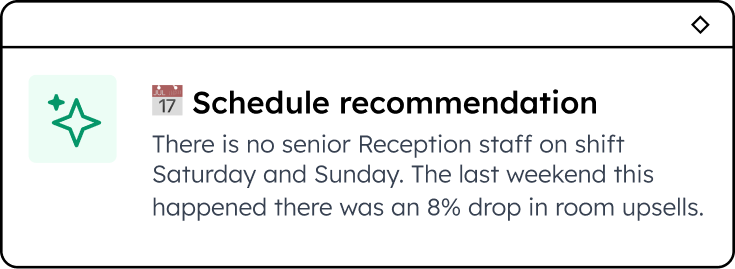
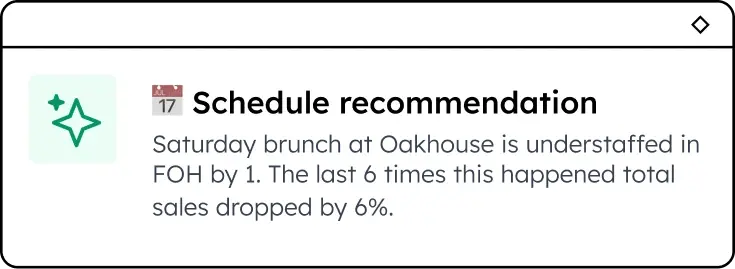
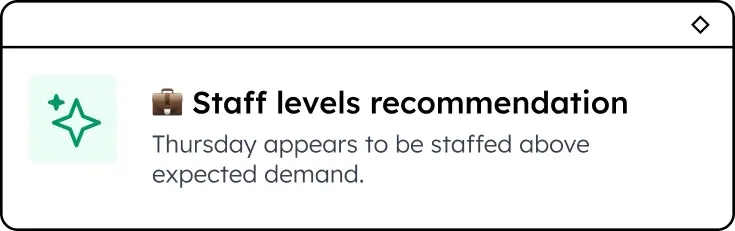
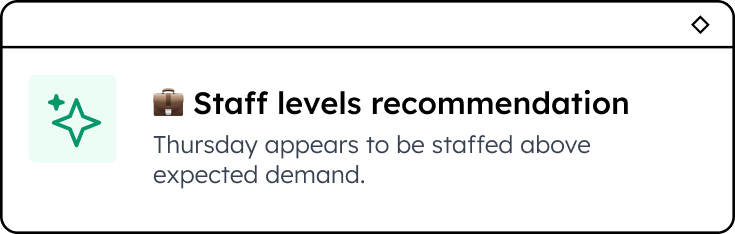
Care providers are also looking into innovative solutions for Workforce Management as a way to increase retention and reduce friction for everyday tasks, allowing care staff to spend less time on admin and more time on care.
It's no surprise that technology is becoming increasingly popular to streamline payroll operations, increase staff engagement and reduce time spent on admin.
‘Workforce shortages across all sectors need to be addressed through innovative initiatives that look to the future. The focus should be on shaping more flexible workforce models that help local systems meet the needs of people – all people – who are in turn empowered to take a more active role in their own wellbeing.’ - Quote from 2022 CQC report.
The recent National Care Awareness Survey 2022 also discovered that 88% of over 600 surveyors would agree that digital technology (like Sona) 'has the power to help reduce workloads and carry out duties faster.'
What’s needed are innovative new ways to relieve some of the strain the health and social care systems are under. With easy-to-use apps like Sona, care workers can optimise their precious time by delegating time-consuming admin jobs to quick, accurate systems, and focusing on other important tasks.
Careful planning and prioritising are the way out of this gridlock, preserving what works and rethinking what doesn’t.
Download our Rethinking Retention report to discover insights and tips to help you retain more staff.
Enjoyed this article? Let's stay in touch 👋
If you liked this article, why not subscribe to our newsletter to get the latest news and views delivered straight to your inbox?