Video: How technology can help care providers reduce staff turnover
Almost 1 in 2 employees in the care sector are considering a role change in 2022.
14 minute read
That was the concerning headline finding from our recent Rethinking Retention report.
In his presentation for UK Care Week, Richard - our Head of Product for Health & Social Care - highlights the key findings and explores how technology can take a leading role in helping employers boost staff engagement, happiness and retention in 3 key areas:
- Scheduling for flexibility (5:50)
- Structuring team communication (10:35)
- Streamlining people processes and data (13:58)
More resources
Discover how Sona can boost employee engagement and retention at your organisation
-
Book a demo with us to speak to one of our knowledgeable and friendly team
-
Check out one of our regular product showcases
-
Got a question? Ask us on live chat (bottom right-hand corner) or drop us a line: hello@getsona.com
Transcript
0:05
Next up, I'm pleased to welcome Richard from Sona who we’re very happy to have as the sponsor of this series. Welcome, Richard.
0:16
Fantastic. Thank you. Gordon and thank you Karolina. That was fantastic and informative. If you'll bear with me, I will need the aid of a powerpoint to get me through this. But don't worry, it shouldn't be too tedious as death by PowerPoint.
0:30
Yes, I'm here from Sona, a technology startup. And in part of our work at the end of 2021, we carried out a survey to get some stats around retention of the care force, not ignoring Covid, but we were focusing on other areas to boost staff engagement and keep staff morale.
So I'm going to share in part some of our findings of our research and talk about the paper, Rethinking Retention, but also go on to look at three key areas that perhaps technology can play a role to try and help keep staff engaged and reduce retention, which is, as Karolina was saying one of the key things that I think we should be focusing on in the industry (very briefly because I don't carry quite the same credentials as the other guest speakers today).
1:19
My name's Richard, I spent the last 10 years working in care. That has included being on the front line, being in the care homes, leading activities, programs for the staff, working with their families as they transition to staying in care homes and then more latterly implementing IT solutions to try and benefit, ultimately the residents, but also the staff.
I've joined Sona within the last 12 months and our product team has grown 200% since I've joined!
1:49
So what we’re doing now is we are creating technology to try and help in the UK care sector. So - Sona - we are a people operating system for care, so we create tools to try and make it easier for staff to have oversight of their shifts, pick up shifts (as Karolina was saying) - the deficit in the workforce at the moment means there's plenty of overtime, there's a lot of extra shifts there.
So it's trying to streamline processes where perhaps staff can pick that up in the easiest way possible if, in fact, they have the capacity and they're able.
Everything we do centres around the employee, we build that first so it's predominantly an app experience.
So an employee can engage with their organization through Sona on their phones to receive that communication from their employer.
2:37
So this goes without saying - this has been covered. Keeping more of your people is a must - with turnover increasing the job vacancy rate is climbing.
And it's not looking better according to our survey. So 44 percent of respondents are considering leaving this year.
That won't all transition to action but that does show some fairly terrifying volume, and a third of those people are looking at leaving the sector entirely. That could be over 200,000 rolls in England alone.
So if there's anything that we can do to chip away, chip away at those numbers, it has to be worth, it has to be worth doing.
3:20
Let me, let me ask, this is a little bit backwards, but let me ask you guys, do you know how much it costs per person to replace essentially. So the churn of each employee. If you do, I don't necessarily need a number.
But I'd be fascinated to hear from those listening. If you can just put in the chat just but a (yes or a y) if you can attribute an actual cost if one of your staff members leaves.
3:46
So the survey..It’s not just about pay. I'm not here to say that care staff shouldn't be paid more. I truly think they do. And again, Karolina touched on that.
But whilst if we accept that there's nothing, well there's certainly nothing I can do about that, then let's look at some of the other factors, that prompt people to change employers.
4:06
It's interesting that out on top is relationships with the residents and patients and that just really goes to show care staff has not stopped caring.
Everybody wants the best, they want to form these close relationships with the people they help, but perhaps what I’ll dwell on a bit more later is number two - more flexible schedules and hours.
62% of our respondents, if they could have more flexible schedule and hours, perhaps would not consider changing employers and I think that's quite powerful.
4:34
And what matters most to staff, you guys can control - and by you guys I mean care home managers, people in head office, even just line managers, it doesn't have to be government funding. It doesn't have to come from that high up. There are small things you can do to champion engagement and make your staff happier.
4:54
Number one - unsurprising I think - but more recognition from management. Something as little as that can have a positive impact on pretty much the entire workforce. And I think after the year, a couple of years that everyone's had in the care industry, that that's very much needed.
5:10
Better internal communication - I think that's very closely tied. I think managers often want to praise their staff, it can be hard to communicate that. It can be hard to get those messages out and make sure that you reach everyone.
5:20
And again we see freedom to choose working patterns crop up, visibility of the schedule. And then again, as Karolina touched, I know the [Care Workers’] charity do great work with mental health for employees in the care sector.
5:33
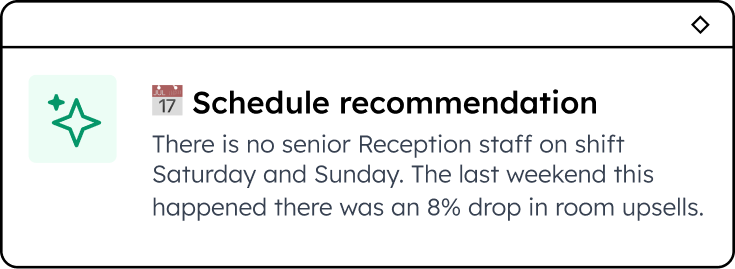
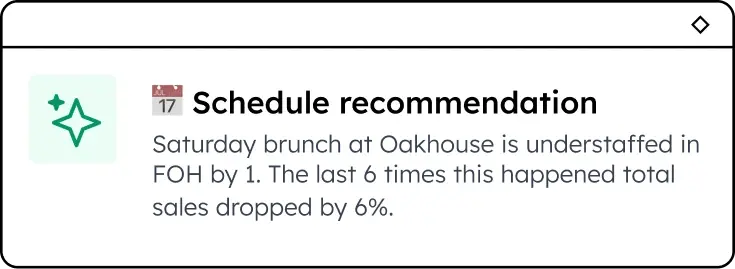
So that's sort of some of the findings from the report. So now let's pivot and look at perhaps some of the ways that tech might be able to help us. So I'm gonna break this into 33 main areas, I'm going to start, sorry, got a bit excited with my slides, with scheduling for flexibility.
5:51
So we've talked about the fact that carers want to care. They want to be in care homes, they want to be looking after the residents, for many of them - over 60% I think - it's more than “just a job”, but they have to do it on terms that suit them and societal and demographic changes.
So long shifts perhaps in care, which we see so often, are maybe becoming less viable as we look at perhaps an older workforce or a pool of people perhaps that are ready for employment that are in later life that might not be liking the idea of 12 hours on their feet and I can't necessarily say I blame them. It's gruelling.
6:29
It's intense but is it possible to put flexibility into the rostering without impacting on the residents and the care that they need? So the main problem as well is engaging, enabling care staff, sorry, to work more flexibly, adds even more complexity to the resourcing and scheduling.
I spent two years in a care home responsible for the schedule. It was a 60 bed care home, we had around 100 staff and it was a nightmare. It's, it's a real challenge.
6:57
And lots of technology providers talk about ‘auto scheduling’ being the solution and it works in theory, if you know how many hours you need to keep your residents safe and if you know how many hours each employee you have hired can do. A computer can fill in those gaps and generate a roster, but there's too many variables - the churn as soon as somebody leaves, which we've talked about, somebody being sick, people being on holiday.
7:26
But more importantly, if a computer is just spitting out hours for someone to work, it's not going to enable them to work when they want, when they can, to be their best selves.
Again, we don't want carers that are exhausted just, as Karolina said, going to work, going to bed, eating, (probably eating before they go to bed) and then back in the next day there needs to be, they need a pattern, they need a work-life balance that works for them whilst enabling them to be in the home doing the job that they love.
7:57
So having a computer spit out when you should work - or even a manager mandating it - isn't necessarily the answer to get the most from your employees. If is there a way to enable employees to work more on their terms. And that's why I believe the solution is moving toward self-scheduling.
8:15
So what is self-scheduling? I don't mean tomorrow you start writing a roster and just ask the care staff to turn up when they want.
That’s not viable, I'm aware of that. But if you, again, if you know what staffing levels you need to be safe or what staffing levels you need to excel - what you need in what role If those shifts are available, perhaps I work 36 hours a week and my manager says to me:
“Here's a fairly fixed schedule - you're going to do these 24 hours every week and the other 12 hours pick up at your leisure. Here's a list of things on an app that you can pick up eight weeks in advance, pick the shifts that you want.”
8:52
So I always get my hours, I always get my money because, you know, that's what's necessary, I need to be working, I need to be earning.
But if I can choose when it's doing it for at least a percentage of my shifts, perhaps that means I can go to my daughter's play recital or I can go to my dentist appointment, silly things that I take for granted now as a sort of work from home employee that can flex my work around my own personal life.
But we should be able to give some of that even to hourly people, hourly paid workers in the care homes. If they could pick up a percentage of their shifts on their terms. We've already seen that can really help boost engagement.
And even overtime shifts - rather than phoning up and invading people's personal lives, which has been happening so much over the last years: “We’re desperate, we need you to come in, we need staff.”
Those phone calls, those WhatsApp messages, are quite intrusive. It's not good for the mental health and mental wellbeing of anyone that's getting them every day around the clock as they need staff.
9:52
If there was a place where all those shifts could go and then a staff member can pick from them - because they want to help.
Again, we've seen this time and time again. Care staff want to come and work and help their colleagues and look after the residents.
So just give them a list that they can tap into and they actually: “Do you know what - Tuesday morning I will go in and I will help out”.
But I haven't had to be badgered by my manager. I haven't had dinner interrupted by a phone call, or my sleep in the event of night staff often I haven't been woken after a shift to be asked to come back in that next night. I can pick it up when I want.
So I think the scheduling for flexibility would be a huge benefit to the workforce, and tech can really help with that and break down some of those barriers.
10:33
The next is structured team communication. So communication is everything, always has been, I think not just in care across the board.
If you're going to manage a good team, you need to be communicating with them at every level. So the rationale here is what we saw earlier in the slides of being recognised for your contributions as the most influential factor for staff morale.
And staff also want to be heard and feel like their views matter. But the problem is when we communicate with staff, certainly in my experience, what I've seen, it's often infrequent and long-form.
There might be a monthly newsletter about things that are going on in the home or things that they need to act on, or more frequent perhaps in the event of covid but still quite long-winded.
That's not the best way. That's not how most people ingest news these days. You think of social media and memes - small, short-form ways of digesting information is going to work perhaps much better.
But without reliable systems in place, it's hard to communicate often and effectively and certainly to a lot of people.
11:35
And when you think that communication needs to be two way, when you're looking for feedback from your staff, that becomes a real challenge.
But if you move away from unstructured forms of communications, can you implement tech to perhaps take some of that burden and also automate it.
So things like surveys - rather than having someone write a long-form survey that you then have to try and get in front of your staff every year or every six months to schedule it.
If you've got maybe two or three questions:
-
“How was your shift?”
-
“How are you feeling?”
-
“Were there any problems?”
12:04
So maybe you’re rating your shift out of five stars, you’re rating how you're feeling out of ‘happy, sad, low’. And then you've got free text for sort of any other business - it could be something as short as that.
And if you schedule that after every shift, or after every five shifts every 10 shifts and it pops up on my phone. I can really quickly think about the volume of data you could capture as a care home manager, or even as a care organisation - someone higher - you could have such an insight into the day that your staff has got and you could be heading off problems and burnout before it's even happened.
Even problems you didn't even know you had - everybody that works on a Tuesday, for instance, starts rating their shift as one star and it transpires perhaps on Tuesdays you have a different chef in and the chef’s really rude to the care staff when they try and serve the residents’ food.
It could be something as small as that has had a massive impact, a massive negative impact, on the care stuff on top of their already stressful, difficult shifts that you didn't know what's happening.
But just by having frequent feedback from the staff, you'd be able to identify things like that and act on it so much quicker, heading off problems before they’re happening. And, again, hopefully reducing churn.
13:11
As for disseminating information. again, you could perhaps just automate a variation of a ‘well done’ message for all your care staff on a regular basis, all your nursing staff, all your hospitality staff, everybody needs and deserves a pat on the back.
13:25
Everyone deserves a well done. Karolina said it all for me earlier - if you can communicate that effectively to your staff, they're going to feel so much better about themselves.
Everyone likes a well done and especially when. and then being able to single out messages yourself and actually said, “You know what, John did a great job today. I saw him with that resident. I just want to pop him a message and make sure that he knows it.”
But technology can enable you to communicate stuff whether you're there in person or not and still try and get that message across.
13:57
So ultimately all of these things are building to streamlining people, processes and data.
If your staff are burnt out now and again - we've seen this - when they reach absolute burnout, they're going to go on sick leave or they're going to quit. And then the problem gets worse and more staff are going to burn out and go on sick leave and quit.
14:13
And so the wheel turns. And better mental health is the most important benefit - again The Care Workers’ Charity touched on that.
And then there's plenty out there in the way of your Fika or Unmind, Calm for Business. There's lots of technology solutions as well to try and help people with their mental health.
14:30
But the problem as we see it is organisations are still far too reactive to this when they see someone burnt out, on sick leave, if they're going to intervene at all, it's normally at that point - and I think we can all agree that that’s too late.
And I think that's just without the data, without a single source of truth, they can't act quick enough.
14:51
I've implemented care management solutions in my time and the reason we implement that is so that we can act on resident behaviour and data before it's a problem.
We know when a resident’s losing weight before they become malnourished. We can identify these sorts of trends and care providers are putting these systems in place in using tech for this for their residents. Why not do it for your staff as well?
15:14
Your staff are just as important at the moment, if not more important. Without staff, without engaged happy motivated staff, you can't look after your residents.
So we really need to start looking at our staff as, as customers and putting the right tech, the right systems in place so that we can do everything in our power to enable them to be happy, be motivated and be the best carers that they can be.
15:40
So I just want to wrap up by talking about implementing tech in care…is daunting having done it for for over five years.
And the very first system I implemented, it was just a learning management system, t was it was just there to be a bit of e-learning for the care staff and I turned up at the pilot home.
I said, “Hi guys, it's Richard from IT, I'm here to show you all about this new system”. And I had a room full of blank faces saying ‘Who? What system? What extra work now?’
And it transpired that no one had told that room full of people that I was coming or what I was talking about. The fact that the people, they've been pulled off their shift or they've been pulled in on their time off, being told “Come in, someone from head office wants to talk to you.”
I mean it's fair to say that was a tense and not a fun hour for me in that room, and that the staff weren't engaged.
16:25
If you're rolling out anything, any new system at all, engage your staff well ahead of time, let them know it's coming, let them feel part of it, let them feel empowered.
Because they are, ultimately, they'll be the end users, you need their buy-in.
16:40
Evaluate what you want from a new piece of tech before you put it in, especially when you can have a pilot or anything like that - have really clear goals. “We want this, this is our problem. We want this tech to come in and fix this problem.”
Give yourself some clear criteria that you can measure against so you can decide was it worth it, was the pilot working?
16:55
And then lastly, don't plough ahead regardless.
If the pilot didn't work, if you didn't see the results that you want, make adjustments. It might be an adjustment of a system, but more likely it's just a different approach.
Talk to the staff that used it, why didn't it go as smoothly as you thought and feel free to tweak your approach before you roll it out.
So if you can engage, evaluate what's happened and then experiment moving forward, we can try and get some decent tech into the hands of all of all care staff.
So that we have ultimately as care managers, a better understanding of what's going on on the floor and hard data that we can act on to help try and lift the morale and boost the engagement of our staff.
Thank you very much
Enjoyed this article? Let's stay in touch 👋
If you liked this article, why not subscribe to our newsletter to get the latest news and views delivered straight to your inbox?